by garnet r. chaney
Garnet's Top Articles
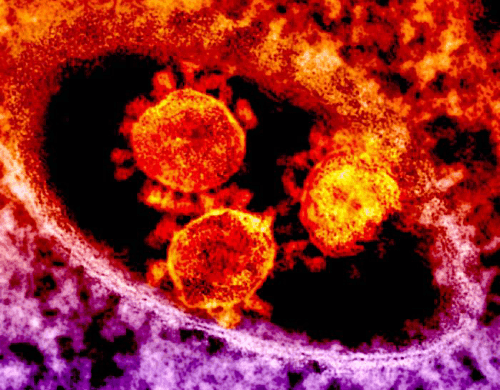
COVID and High Blood Pressure and drugs used for its treatment
I have been watching closely for articles on any link between the lisonopril side effect of dry hacking cough, and COVID mechanism of attack on the lungs.

TheGarnet's Wiki
My wiki is a primary place where I keep track of my latest research on various issues. In the wiki, you can join the discussion and contribute to the research.
Who Sharpens Your Shears?
Garnet providees premium beauty shear sharpening in the San Francisco Bay Area.